Our Books

Title: The Mystery of Medicine: The Autonomic Nervous System Dysfunction
Abstract: The autonomic nervous system in our body adapts to changes in the internal and external environment and controls vital structures such as the heart, vessels, intestines, and reproductive organs in our body. It mainly consists of two components: the sympathetic system, which causes the “fight or flight” response, especially in the presence of danger, a threat or in a state of panic, etc.; and the parasympathetic nervous system, whose intrinsic properties shortly referred to as “rest and digest” help to calm down the body, allow growth and development and lower the level of stress.
As the stress factors in our routine life rise, the autonomic nervous system dysfunction may cause numerous disorders and diseases including depression, headaches, gastrointestinal disorders, sleep problems, cardiac problems, and etc. Understanding the autonomic nervous system and its dysfunctions will actually increase your awareness with regard to these problems, and potential solutions.
Author: Ali Veysel Özden, M.D., Ph.D.
Title: Vagus Nerve Stimulation
Contents:
- Acute Effects of Vagal Neuromodulation Approaches in Healthy Individuals
- A Review on the Effect of Vagus Nerve Stimulation on Brain Frequency Bands
- The Effect of Bilateral Transcutenous Auricular Vagus Nerve Stimulation on Working Memory and Neuropsychiatric Profile
- The Impact of the Vagus Nerve on Neurodegenerative and Neuropsychiatric Conditions in Connection with the Oral and Intestinal Microbiome
- Effects of Non-invasive Vagus Nerve Stimulation on Behavioral, Physiological, and Neural Responses to Food in Humans: A Traditional Review
- The Effects of Diet Content on the Vagus Nerve
- Personalized Auricular Non-invasive Vagus Nerve Stimulation System for Inflammatory Bowel Disease Treatment
- Vagus Nerve Stimulation and Pregnancy
- Nursing Roles and Responsibilities in Vagus Nerve Stimulation
- Vagus Nerve Stimulation in School Nurses’ Epilepsy Management: Why is it Necessary to Know?
- The Role of the Vagus Nerve in Rheumatoid Arthritis
Our Articles and Clinical Researches
Title:Morphometric Changes in Liver and Pancreas in Experimental Colitis Model and Examination of the Effects of Vagal Stimulation on These Changes in Chronic Period
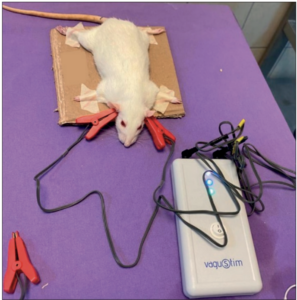
Introduction: Inflammatory bowel disease is a chronic and idiopathic disease of the digestive tract. The disease also affects the liver and pancreas. Our aim in the study was to examine the effect of transcutaneous auricular vagal nerve stimulation (TAVNS) on the healing of liver and pancreas damage.
Material and Method: 36 rats in 4 groups were included in this study. The Sham group was intracolonic injected with saline and TAVNS was not applied. The Sham+ TAVNS group was injected intracolonically with saline and TAVNS was applied. The TNBS+Sham group was injected with TNBS (trinitrobenzene sulfonic acid) intracolonically and TAVNS was not applied. In TNBS+ TAVNS group, both TNBS was injected and TAVNS was applied. Liver tissue and pancreas tissue were examined histologically and histomorphometrically. Results: In our study, the final body weights of TNBS+Sham and TNBS+ TAVNS groups were found to be significantly lower than Sham and Sham+TAVNS groups. The liver and pancreas histopathological scores of the TNBS injected groups were significantly higher. In the liver hepatocytes of rats in TNBS+Sham group, necrotic areas, vacuolar degeneration, and sinusoidal congestion were observed in some regions. Degenerative findings in liver sections of group TNBS+ TAVNS group were also partially reduced. The number and area of Langerhans islets in the pancreas of the animals in TNBS+Sham and TNBS+ TAVNS groups were found to be lower than in Sham and Sham+ TAVNS groups.
Conclusion: In this study, we found that TNBS-induced colitis in rats caused histopathological and histomorphometric changes in the liver and pancreas, causing weight loss, and that TAVNS had therapeutic effects on these changes.
Keywords: Colitis, vagal nerve stimulation, liver, pancreas
Title: Comparison of the efficacy of auricular vagus nerve stimulation and conventional low back rehabilitation in patients with chronic low back pain
Background: In recent years, human and animal studies have provided increasing evidence that vagus nerve stimulation (VNS) can produce analgesic effects as well as alleviating resistant epilepsy and depression. Our study was designed to compare the efficacy of transcutaneous auricular vagus nerve stimulation with conventional low back rehabilitation in patients with chronic low back pain (CLBP).
Methods: Sixty patients with LBP were randomly divided into two groups. Group 1 received conventional rehabilitation and home exercise, and Group 2 received transcutaneous auricular VNS and home exercise. Both groups received treatment five days a week for three weeks. Trunk mobility (Modified Schober test, fingertip-to-floor test), muscle strength (CSMI-Cybex Humac-Norm isokinetic dynamometer and Lafayette manual muscle strength measuring device), trunk endurance, balance tests, Visual Analog Scale, Beck Depression Scale, Pittsburgh Sleep Quality Index, Oswestry Disability Index were evaluated.
Results: At the end of three weeks, within-group assessment results showed positive effects on mobility, functional status, depression and sleep in all groups (p < 0.05). Pain level, endurance time and flexion trunk muscle strength results showed more improvement in Group 2 (p < 0.05). Some parameters of isokinetic lower extremity quadriceps muscle strength and fall risk scores showed a significant improvement in Group 1 (p < 0.05).
Discussion: VNS has been observed to be more effective on pain, trunk muscle strength and endurance duration and sleep status. Auricular VNS may be included in the treatment of patients with CLBP in whom conventional physical therapy is inadequate or not applicable.
Keywords: Autonomic nervous system; Low back pain; Vagus nerve stimulation.

Title: Effects of Auricular Vagus Nerve Stimulation on Cardio-Respiratory Functions After Aerobic Exercise
Abstract: The aim of our study is to find out whether the return rate of parasympathetic activity (PA) can be accelerated with auricular transcutaneous vagus nerve stimulation (TVNS). Pulmonary function test, ANS activity, pulse and blood pressure measurements were made. Individuals ran for 15 minutes. Those in the TVNS group received 5 minutes of auricular VNS. In the control group, headphones were attached but no current was given. After the end of their procedures, they were compared with pre-exercise. In the TVNS group, the pulse parameter was higher than in the initial measurement (p=0.001). There was a significant (p=0.007) rise in the FEV1 value in the VNS group. The sympathetic nervous system (SNS) index (p<0.05) increased in both groups when compared to the initial measurement, although there was no significant difference in the index values between the groups. The TVNS group showed an increase from the first measurement (p<0.05), but there was no significant difference in the parasympathetic nervous system (PNS) Index between the groups (p>0.05). The groups’ values for the first and second measures were equal (p>0.05), and the root mean square of the successive differences (RMSSD) values did not reveal a significant difference. TVNS can improve respiratory parameters in healthy individuals in the acute period after exercise, and it seems that it can also increase activation in both the sympathetic and parasympathetic system. It can be stated that TVNS may lead to variable results in different circumstances in sports.
Keywords Vagus Nerve, Stimulation, Respiratory Function, Exercise Recovery
Title: Personalized Auricular Non-invasive Vagus Nerve Stimulation System for Inflammatory Bowel Disease Treatment
Abstract: Inflammatory bowel disease (IBD) is a chronic relapsing clinic condition whose cure could be very difficult even with new treatments. Although tremendous changes have occured in IBD treatment; there is an unmet need for a low-cost, easy-to-access treatment associated with low side effects. Possible dysfunction of interaction between the microbiome-gut-brain axis and autonomic nervous system; expecially vagus nerve dysfunction can be targeted for a new therapy. Given this, vagus nerve stimulation (VNS) camoes to the fore. Using present literature, we reviewed pathophysiology of IBD and anti inflammatory effect of VNS and the current aim of this review is to provide a comprehensive understanding of the effect of VNS on gut inflammation and the potential of personalized auricular VNS on IBD management. In the field of precision medicine these days, when digital transformation in health comes to the fore, personalized auricular VNS which uses machine learning algortims may be an complementary treatment of IBD.
Keywords: Autonomic nervous system; complementary medicine; inflammatory bowel disease; vagus nerve stimulation
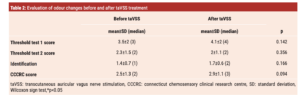
Title: The Effects of Transcutaneous Auricular Vagus Nerve Stimulation on Nerve Conduction Velocity, Grip Strength, Pain, and Upper Extremity Functionality in Individuals with Carpal Tunnel Syndrome
Purpose: This study aims to investigate the effects of transcutaneous auricular vagus nerve stimulation (taVNS) on key parameters, including nerve conduction velocity, grip strength, pain, and upper extremity functionality in individuals with carpal tunnel syndrome (CTS).
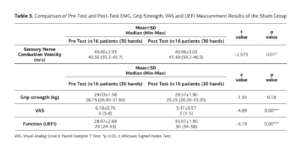
Methods: The study involved 51 patients (90 hands) diagnosed with carpal tunnel syndrome, comprising 12 males and 39 females, ranging in age from 18 to 58 years. Participants were divided into groups by random randomization method. Sensory branch conduction velocity of the median nerve was assessed via electromyography (EMG), hand grip strength was measured using a digital dynamometer, and pain intensity was quantified with a visual analog scale (VAS); additionally, upper extremity functionality was evaluated using the Upper Extremity Functional Index (UEFI) scale before and after the treatment. In the experimental group, in addition to the conventional physiotherapy program, 10 sessions of auricular vagus nerve stimulation were administered; for the sham and control groups, the conventional physiotherapy program alone was conducted over the course of 10 sessions.
Results: The analysis revealed no statistically significant differences between the groups concerning variables such as body mass index (BMI), age, gender, educational background, and smoking status (p>0.05). However, within-group evaluations exhibited significant differences compared to baseline values in terms of nerve conduction velocity, pain perception, and upper extremity functionality, with no such difference observed in grip strength (p<0.05). The intergroup comparisons indicated a significant difference in favor of the experimental group across all parameters, except for grip strength (p<0.05); conversely, no substantial differences were observed between the sham and control groups (p>0.05).
Conclusion: The findings suggest that the adjunctive use of taVNS alongside conventional rehabilitation programs in individuals diagnosed with CTS results in increased sensory nerve conduction velocity and enhanced upper extremity functional capacity, accompanied by a reduction in pain; nevertheless, grip strength remains unaffected.
Keywords: Cranial Nerve X, Carpal Tunnel, Nerve Conduction Studies
Title: The Effects of Transcutaneous Auricular Vagus Stimulation on Sustained Attention and Depression in Individuals Who Are Likely to Have ADHD
Aims: This study aims to evaluate the effects of transcutaneous auricular vagus nerve stimulation (taVNS) on sustained attention and depression in individuals with suspected attention deficit hyperactivity disorder (ADHD).
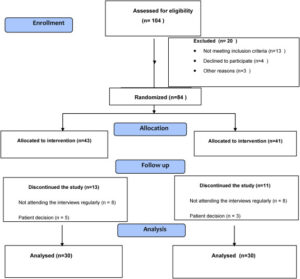
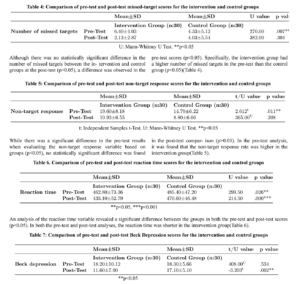
Methods: Between May 1, 2022 and September 25, 2022, the study included 60 students (9 males, 51 females; mean age: 21.11±1.6 years; range, 18 to 24
years) identified as being at high risk for attention deficit hyperactivity disorder (ADHD). Participants were randomly assigned to either the intervention or control groups. Each group consisted of 30 individuals. The intervention group received taVNS in conjunction with mobile-assisted games and relaxation exercises, while the control group received mobile-assisted games and relaxation exercises alone. The data were collected using a descriptive information form, the Beck Depression Inventory, and mobile-assisted assessment parameters. Data were analyzed using the Wilcoxon signed-rank test, t-test, and MannWhitney U test. Results: Significant differences were observed in the intervention group concerning the sub-parameters used to measure attention and depression scale scores; however, in the control group, all but one of the attention sub-parameters showed significant differences. A comparison between the two groups revealed significant differences in reaction times and Beck Depression Inventory scores in favor of the intervention group.
Conclusion: This study revealed that taVNS can effectively
improve attention (cognitive function) and alleviate symptoms of depression.

Title: Acute Effect of Transcutaneous Auricular Vagus Nerve Stimulation on Hand Tremor in Parkinson’s Disease: A Pilot Study of Case Serie
Objectives: The aim of this study is to investigate the effects of non-invasive vagus nerve stimulation (VNS) on tremor in Parkinson’s disease (PD)
Methods: This single-center, prospective, and implementation study with before-after design included five participants diagnosed with PD. Auricular VNS was applied to each participant 3 times on different days. VNS was applied to the participants as the right ear, left ear, and bilateral ear. The cardiovascular parameters of the participants were evaluated with Kubios HRV Standard and tremor with UPDRS tremor subscale and smartphone application before and after the intervention
Results: A significant decrease in diastolic blood pressure (p=0.043) was found in participants who underwent bilateral auricular VNS. Although there was no significant change in the UPDRS tremor subscale, decreases in the maximum tremor amplitude in the x (p=0.043) and y (0.014) planes were detected in the measurements made with the smartphone application.
Conclusion: In this study, a decrease in the tremor amplitude measured in the 3D plane with auricular VNS was found in patients with PD.
Authors: Ahmet Kivanc Menekseoglu, Merve Damla Korkmaz, Enes Efe Is, Ceyhun Basoglu, Ali Veysel Ozden
Keywords: Parkinson’s disease; tremor; vagus nerve stimulation.
Title: Non-invasive vagus nerve stimulation in a hungry state decreases heart rate variability
Abstract: Vagus nerve signals from the gut to brain carry information about nutrients and drive food reward. Such signals are disrupted by consuming large amounts of high-calorie foods, necessitating greater food intake to elicit a similar neural response. Non-invasive vagus nerve stimulation (nVNS) via a branch innervating the ear is a candidate treatment for obesity in humans. There is disagreement on the optimal location of nVNS in the ear for experimental and clinical studies. There are also no studies comparing nVNS in hungry and post-prandial states. We aimed to compare ear position(s) for nVNS and explore the effects of nVNS during hungry and post-prandial states on proxies for autonomic outflow (heart-rate variability) and efferent metabolism (gastric wave frequency and resting energy expenditure). In a within-subject design, 14 participants (10 women, on average 29.4 +/- 6.7 years old) received nVNS in four different locations (cymba conchae, tragus, earlobe, or tragus AND cymba conchae) on separate days. In each session, participants were asked to consume a palatable chocolate flavored milk. With electrography on the abdomen and indirect calorimetry in a canopy, we measured electro-cardiogram, electro-gastrogram and resting energy expenditure for 15 min before and at least 35 min after consumption of the palatable drink. We also collected ratings of the palatable drink and internal and other states. Pre-drink consumption (in a hungry state) we observed no differences in the effect of location of acute nVNS on resting energy expenditure and gastric wave measures. However, nVNS in cymba conchae decreases heart-rate variability (relative to sham) and ratings of how much participants want to consume the drink (relative to tragus AND cymba conchae and a trend relative to sham). After drink consumption and with continued nVNS, gastric wave frequency is unchanged, and resting energy expenditure increases regardless of stimulation location. Heart-rate variability decreases in all locations, except cymba conchae. We also observe a trend for an increase in gastric wave amplitude in late post-drink consumption time-points in cymba conchae. We observe no support for the combined stimulation of tragus AND cymba conchae being more effective than either of the individual locations. These results suggest that nVNS in the cymba conchae in a hungry state has a similar acute effect on vagal tone as food consumption: to decrease heart rate variability. This effect then negates the usual postprandial effects of a decrease in heart rate variability as seen in the other nVNS locations. These preliminary observations suggest that nVNS in cymba conchae may act primarily on vagal afferent autonomic (and only modestly on metabolic output) in a similar way as food consumption does.
Authors: Zeynep Altınkaya, Lina Öztürk, İlkim Büyükgüdük, Hüseyin Yanık, Dilan Deniz Yılmaz, Berçem Yar, Evren Değirmenci, Uğur Dal, Maria Geraldine Veldhuizen
Keywords: Electrogastrogram; Energy expenditure; Food reward; Heart-rate variability; Transcutaneous auricular vagus nerve stimulation; Wanting.

Title: Effects of a single session of noninvasive auricular vagus nerve stimulation on sports performance in elite athletes: an open-label randomized controlled trial
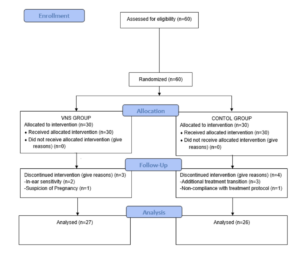
Objectives: The purpose of this study was to investigate the efficacy of noninvasive auricular vagus nerve stimulation (AVNS) on sports performance.
Methods: The intervention group (n = 30) received a single session of AVNS, while the control group (n = 30) received a single session of sham AVNS. Pre- and post-treatment isometric quadriceps muscle strength, heart rate, lower extremity balance, and grip strength were measured.
Results: It was ascertained that the differences in heart rate (-0.73 pulse/min, p = 0.032) and modified Star Balance Test scores (anterior 2.72 cm, p = 0.000, posterolateral 3.65 cm, p = 0.000 and posteromedial 2.43 cm, p = 0.000) before and after AVNS were significant in subjects in the experimental group. The results of the one-way ANOVA analysis show that the differences obtained in all measurement parameters are not statistically significant (p > 0.05). Considering the partial eta squared (η2) obtained from the measurements, a small descriptive effect in favor of experimental group was obtained for the quadriceps strength (0.016) and anterior balance (0.054) measurements.
Conclusion:This study demonstrates that a single AVNS session compared to sham AVNS shows a modest benefit though not statistically significant improvement in athletic performance. Single-use of AVNS seems not effective in improving athletic performance.
Authors: Adem Çalι, Ali Veysel Özden, İsmail Ceylan
Keywords: Auricular vagus nerve stimulation; balance; performance; recovery; strength.

Title: A54 THE IMPACT OF NON-INVASIVE TRANSCUTANEOUS AURICULAR VAGUS NERVE STIMULATION (NITAVNS) ON THE DEVELOPMENT OF EXPERIMENTAL COLITIS IN MICE
Background: The anti-inflammatory impacts of stimulating the vagus nerve as a part of the gut-brain axis on intestinal macrophage activity and inflammatory cytokine production have been documented. While vagus nerve stimulation until now has been chiefly invasive, non-invasive auricular vagus nerve stimulation (NitaVNS) has no adverse effects associated with invasive stimulation. The NitaVNS-mediated activation of brainstem nuclei can exert anti-inflammatory effects directly on the colon or indirectly through the spleen via a macrophage-acetylcholine-dependent pathway.
Methods: Thirty C57BL/6 mice aged 11 to 12 weeks were divided into four groups: control (CTRL)-NitaVNS, CTRL-Sham, dextran sulphate sodium (DSS)-NitaVNS and DSS-Sham. Pre-set stimulation parameters (10 minutes duration, 10 V voltage, 500 s pulse width, and 20 Hz frequency) were applied for NitaVNS or sham-paw stimulation. 5% DSS was administered to induce colitis for five consecutive days, whereas CTRL mice received regular water. Weight loss, stool consistency, blood in the feces, and disease activity index were evaluated daily. Rectal bleeding, colon bleeding, and fecal consistency were determined as a composite macroscopic score upon sacrifice. Collected colon and blood samples were assessed for pro-inflammatory parameters such as interleukin (IL)-1β, tumor necrosis factor (TNF)-α, IL-6, C-reactive protein (CRP), matrix metalloproteinase (MMP)-2, macrophage inflammatory protein (Mip)-1α and β, and anti-inflammatory cytokine tumor growth factor (TGF)-β using qRT-PCR and ELISA.
Results: Compared to colitic-sham mice, colitic NitaVNS mice demonstrated a delayed onset and a significantly lower clinical disease severity. Colitis induced significant weight loss, rectal bleeding, and stool consistency loss, and NitaVNS significantly abolished these effects. In colitic conditions, NitaVNS decreased the disease activity index significantly compared to the colitic sham group. Colitis increased the macroscopic scores, and NitaVNS decreased them significantly. Conversely, colon length was significantly reduced in colitic conditions, but NitaVNS abrogated that deleterious effect. mRNA expression levels of IL-1β and TNF-α were significantly increased in colitic mice and NitaVNS decreased them significantly. Whereas Mip-1α and 1β were not modified in colitic conditions, NitaVNS significantly decreased these markers. MMP2 mRNA expression and colonic IL-6 and IL-1β protein levels were not altered in all conditions. However, colitis induced a significant decrease in colonic TGF-β levels, but NitaVNS did not amplify that effect. Interestingly, in the serum of colitic mice, NitaVNS significantly increased and decreased TGF-β and CRP levels, respectively.
Conclusion:These findings suggest that NitaVNS possess some spatial anti-inflammatory effects in acute colitis through the up or downregulation of anti- or pro-inflammatory markers.
Authors: F Hesampour, D Tshikudi, A Veysel Özden, C N Bernstein, J -E Ghia
Keywords: colitis, vagus nerve stimulation.

Title: The effects of transcutaneous auricular vagus nerve stimulation on visual memory performance and fatigue
Objectives: This study aims to investigate the effects of transcutaneous auricular vagus nerve stimulation (taVNS) on visual memory performance and fatigue in healthy individuals.
Methods: Between April 10, 2022 and May 25, 2022, a total of 60 physical therapy and rehabilitation students (27 males, 33 females; mean age: 20.6±1.6 years; range, 18 to 24 years) were included in the study. The individuals were divided into two groups as the experimental group (n=30) and the control group (n=30). The experimental group received taVNS, mobile device supported games, and low-medium intensity aerobic exercises, while the control group received mobile device supported games and aerobic exercises. The personal information form was applied to all participants. The level of fatigue was measured using a computer-based evaluation and Fatigue Severity Scale (FSS) to analyze the visual memory performance.
Results: All parameters used to evaluate visual memory performance showed a significant difference, while the FSS scores showed no significant difference (p>0.05). Only one sub-parameter in the control group was significantly different, while none of the other sub-parameters or FSS scores were significantly different (p>0.05). There was a significant difference between the two groups in terms of two of the visual memory sub-parameters, although no significant difference was found for the results of one parameter and the FSS (p>0.05).
Conclusion: Our study results show that taVNS can produce positive effects on visual memory performance, although it does not apparently affect fatigue.
Authors: Rıdvan Yıldız, Ali Veysel Özden, Onur Seçgin Nişancı, Zeynep Yıldız Kızkın, Bedriye Cansu Demirkıran
Keywords: Fatigue; transcutaneous auricular vagus nerve stimulation; visual memory.

Title: A New Method for Sportive Performance and Recovery: Auricular Vagus Nerve Stimulation (Review)
Abstract: During sports and exercise, the cardiovascular system, respiratory system, musculoskeletal system, nervous system, endocrine system, and immune system play an active role. With the start of exercise, sympathetic activity in the body increases and parasympathetic activity is suppressed. With the end of the exercise, sympathetic activity decreases, while parasympathetic activity increases and contributes to the recovery process of the individual. The contribution of the parasympathetic system to the restructuring/recovery during the rest period is important in terms of reducing the fatigue of the athletes and enabling them to recover in the early period. Stimulation of the vagus nerve, which is the main branch of the parasympathetic system, can affect many cardiovascular, pulmonary, and metabolic parameters both during rest and exercise. Our article aims to evaluate the potential benefits and effects of using auricular vagus nerve stimulation (VNS) for sports purposes on the recovery and performance of athletes in light of the literature. Recovery after exercise can be accelerated with auricular VNS. The negativities caused by overload and excessive training can be reduced. Thanks to better rest and early recovery, the performance in the following training program can be increased. Injuries that may occur due to insufficient recovery can be prevented or injuries can be reduced. We can expect that the auricular VNS method will be used soon in light of sufficient scientific data due to its effects that cannot be considered doping.
Authors: Ali Veysel Özden, Kerem Alptekin, Mehmet Unal

Title: Effects of Auricular Vagus Nerve Stimulation on Voice Characteristics
Abstract: Vagus nerve stimulation (VNS) has been used in the treatment of epilepsy and depression for more than 20 years. Although the invasive cervical method is the most preferred application, side effects such as cough, voice change and hoarseness can be seen due to negative effects on the recurrent laryngeal nerve (a branch of the vagus nerve). Auricular VNS has been preferred recently due to its non-invasiveness, but uncertainty about the stimulation parameters continues. We tested the hypothesis that auricular VNS can affect voice and its features indirectly via afferent nerve connections reaching the nucleus tractus solitarius. Two patients previously using auricular VNS device for different diseases were requested to record their voices before and after the stimulation. Their devices (Vagustim) were changed with new version to check the usage of the patients. Sound recordings at different VNS frequencies (1-150 Hz) were collected by a mobile phone and analyzed with Praat and our MATLAB algorithm. Fundamental frequency (f0), jitter, shimmer, and harmonic to noise ratio (HNR) owere evaluated. The alteration was highest at 100 Hz and 30 Hz VNS for the male and female patients respectively. Audio recordings before and after 30 Hz (for female) and 100 Hz (for male) VNS at different durations (5-30 min) on different days were repeated and compared by Praat and our algorithm. Some discrepancy between the parameters jitter, shimmer, and HNR are detected between the algorithms, which is accounted to the fact that it is not standardized whether the algorithm uses only a specific part of the input signal or the whole signal. However, when the ratio of change of these parameters are considered, fundamental frequency and the HNR were found to be highly consistent for developing an algorithm to govern the stimulation parameters in an automated way. Furthermore, the same ratios for jitter and shimmer are also promising after some improvement to be included in such an algorithm. These results suggest that auricular VNS can affect voice and its parameters, but this change is related with stimulation parameters. It seems necessary to develop specific software and algorithms that can detect this change well.
Authors: Ali Veysel Özden, Tayfun Tatar

Title: Acute Effect of Auricular Vagus Nerve Stimulation on Cycle
Ergometer Test and Physiological Parameters in Healthy
Young Individuals: A Pilot Study
Background: This study is to investigate the effect of non-invasive auricular VNS on cycle ergometer test and physiological parameters in healthy individuals.
Methods: 46 people participated in the study. The participants were randomly divided into 3 groups as Above Threshold, Under Threshold and Control according to the sensation of electrical current on ears. The participants were evaluated 3 times; before the application, after the first and second bicycle exercises. Numerical pain scale, pulse rate, blood pressure, respiratory rate, and distance travelled during exercise for cycle ergometer test.
Results: There was no significant difference in 1st measurement, 2nd measurement, 3rd measurement of pulse rate, saturation value and performance in the control group, sub-threshold group and above threshold group (p ˃ 0.05). The 2nd measurement of NPS value was significantly lower in the above threshold group than in the control group and the below threshold group (p ˂ 0.05). The 1st measurement, 2nd measurement, 3rd measurement respiratory rate and 3rd measurement diastolic pressure values were significantly higher in the sub-threshold group (p ˂ 0.05).
Conclusion: In healthy individuals, short-term non-invasive auricular VNS does not affect cycle ergometer test during exercise. This may be due to the fact that the application time is kept short and the application is a single time. In VNS application, feeling the current and/or current intensity may affect parameters such as respiratory rate and blood pressure.
Authors: Sefa Haktan HATIK, PT, Berkay Eren Pehlivanoğlu, Mesut ARSLAN, Çilem TAŞKIN, and Ali Veysel ÖZDEN
Title: Short-term effectiveness of auricular vagus nerve stimulation in patients with myofascial pain syndrome
Objectives: To evaluate the effect of auricular vagus nerve stimulation (VNS) applied in addition to ischemic compression and stretching exercises on pain, trigger point (TP) sensitivity, grip strength, quality of life and autonomic functions in patients with myofascial pain syndrome (MPS).
Methods: Sixty patients, who had neck pain, met the diagnostic MPS criteria of Travell and Simons were included in the study. The subjects were randomly divided into VNS group (n = 30) or control group (n = 30). Each group performed 10 sessions of TP ischemic compression and stretching exercises (5 days/week). Ten sessions of 30-minute long auricular VNS were added to the treatment in VNS group. Pain severity [Visual Analogue Scale (VAS)], TP sensitivity (algometer), grip strength (Jamar dynamometer), quality of life [Short Form-36 (SF-36)] and autonomic function [Composite Autonomic Symptom Scale-31 (Compass-31)] were evaluated before and after 10 sessions of treatment.
Results: The VAS, algometer and Jamar measurements showed significant improvement in both groups. A statistically significant improvement was found in orthostatic intolerance, secretomotor and pupillomotor subscales of Compass-31 scale in the VNS group following the treatment (p < 0.05) while no significant difference was observed in the control group (p > 0.05). The control group showed significant improvement in all parameters of SF-36 scale, while the VNS group showed significant improvement in physical function, social functionality and pain parameters (p < 0.05). The changes in the VAS, algometer, Jamar scores and secretomotor subscale of the Compass-31 scale were statistically higher in the VNS group than in the control group (p < 0.001, p < 0.001, p = 0.001 and p = 0.011, respectively).
Conclusions: It can be argued that auricular VNS increases the effectiveness of ischemic compression and stretching exercises in patients with MPS. Further and detailed studies are needed in which the effect of VNS alone or in combination with other treatments in patients with MPS is examined and the physiological mechanisms are investigated.
Keywords: Myofascial pain syndrome, auricular vagus nerve stimulation, ischemic compression, autonomic nervous system, quality of life
Authors: Simay Ünal, Dilber Karagözoğlu Çoşkunsu, Sefa Haktan Hatık, Ali Veysel Özden
Title: The Effect of Vagus Nerve Stimulation Applications on Taste and Smell Loss in COVID-19 Syndrome: Case Report
Abstract: Loss of the sense of taste and smell is a common side effect of Covid 19. It is thought that transcutaneous ear vagus nerve stimulation may affect taste and smell as a result of neural connections. We present a 27-year-old female participant diagnosed with loss of taste and smell for more than 1 year. The Connecticut Chemosensory Clinical Research Center (CCCRC) olfactory test was used to test the sense of smell. To test the sense of taste, 3 drops of taste test were applied. It was found that during the application period of 1 session per day for 15 days, there was a progressive improvement in the sense of taste and smell.
Authors: Berkay Eren Pehlivanoglu , Sanem Guven , Sefa Haktan Hatik , Ali Veysel Ozden

Title: The effect of auricular vagus nerve stimulation on electroencephalography and electromyography measurements in healthy persons.
Objectives: Auricular vagus nerve stimulation (VNS) is a non-invasive treatment
modality. Opinions that it can be used in the treatment of various clinical problems
have gained importance in recent years. In this study, it was aimed to lay the
groundwork for the use of the auricular VNS in different ears.
Methods: Healthy individuals (n = 90) were divided into three groups: unilateral
left (n = 30), unilateral right (n = 30), and bilateral (n = 30) auricular VNS.
Electroencephalography (EEG) and electromyography (EMG) measurements
were performed before and after auricular VNS (10 Hz, 300 μs, 20 min) for a
single session.
Results: An increase in wrist extensor muscles activation was detected on the
contralateral side of the auricular VNS application side. It has been observed that
there is a general decrease in the power of high-frequency waves and an increase
in the power of lower-medium frequency waves in various parts of the brain.
Conclusion: Our findings suggest that the projection of the auricular VNS in the
central nervous system may also affect the corticospinal tracts.
Authors: Gülşah Konakoğlu, Ali Veysel Özden, Hakan Solmaz, Celaleddin Bildik4
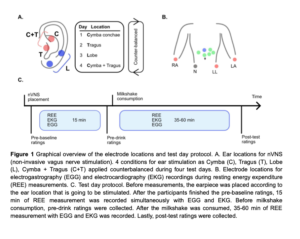
Title: Non-invasive vagus nerve stimulation in a hungry state decreases heart rate variability and wanting of a palatable drink
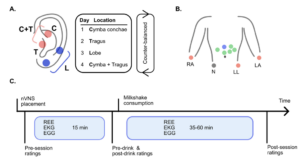
Abstract: Vagus nerve signals from the gut to brain carry information about nutrients and drive food reward. Such signals are disrupted by consuming large amounts of high-calorie foods, necessitating greater food intake to elicit a similar neural response. Non‐invasive vagus nerve stimulation (nVNS) via a branch innervating the ear is a candidate treatment for obesity in humans. There is disagreement on the optimal location of nVNS in the ear for experimental and clinical studies. There are also no studies comparing nVNS in hungry and full states. We aimed to compare ear position(s) for nVNS and explore the effects of nVNS during hungry and full states on proxies for autonomic outflow (heart-rate variability) and efferent metabolism (gastric frequency and resting energy expenditure).
In a within-subject design, 14 participants (10 women, on average 29.4 +/- 6.7 years old) received nVNS in four different locations (cymba conchae, tragus, earlobe, or tragus AND cymba conchae) on separate days. In each session, participants were asked to consume a palatable chocolate flavored milk. With electrography on the abdomen and indirect calorimetry in a canopy, we measured electro-cardiogram, electro-gastrogram and resting energy expenditure for 15 minutes before and at least 35 minutes after consumption of the palatable drink. We also collected ratings of the palatable drink and internal and other states.
Pre-drink consumption (in a hungry state) we observed no differences in the effect of location of acute nVNS on resting energy expenditure and gastric frequency. However, nVNS in cymba conchae decreases heart-rate variability and ratings of how much participants want to consume the drink. After drink consumption and with continued nVNS, gastric frequency is unchanged, and resting energy expenditure increases regardless of stimulation location. Heart-rate variability decreases in all locations, except cymba conchae. We also observe a trend for an increase in gastric frequency in late post-drink consumption time-points in cymba conchae. These results suggest that nVNS in the cymba conchae in a hungry state has a similar acute effect on vagal tone as food consumption: to decrease heart rate variability. This effect then negates the usual postprandial effects of a decrease in heart rate variability as seen in the other nVNS locations. This suggests that nVNS in cymba conchae may act primarily on vagal afferent autonomic (and only modestly on metabolic output) in a similar way as food consumption does.
Authors: Zeynep Altınkaya, Lina Öztürk, İlkim Büyükgüdük, Hüseyin Yanık, Dilan Deniz Yılmaz, Berçem Yar, Evren Değirmenci, Uğur Dal, Maria Geraldine Veldhuizen
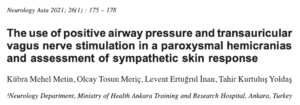
Title: The use of positive airway pressure and transauricular vagus nerve stimulation in a paroxysmal hemicranias and assessment of sympathetic skin response
Abstract: Paroxysmal hemicrania is characterised by severe short-term unilateral headaches that are associated with ipsilateral cranial autonomic symptoms. A rare headache type, paroxysmal hemicrania is included in the trigeminal autonomic cephalgia group of primary headache. The relationship between paroxysmal hemicrania and sleep apnoea has not been previously reported in the literature. Noninvasive vagus nerve stimulation offers an alternative treatment option for patients who cannot tolerate indomethacin or other traditional treatments. We report the case of a female patient with sleep apnoea and paroxysmal hemicrania who could not use indomethacin and other therapies. Her headaches temporarily regressed with positive airway pressure treatments and positively responded to transauricular vagus nerve stimulation. We evaluated the stimulatory effect of this treatment by examining the patient’s sympathetic skin responses.
Authors: Metin, Kübra Mehel; Meriç, Olcay Tosun; İnan, Levent Ertuğrul; Yoldaş, Tahir Kurtuluş

Objective: The aim of this study is to investigate the effect of non-invasive auricular VNS (Vagus Nerve Stimulation) on sportive performance and physiological parameters in healthy individuals.
Material and Method: 46 healthy young individuals aged 19.2(±1.5) years participated in the study. The participants were randomly divided into 3 groups as Above Threshold Group (n:15; 10 females, 5 males), Under Threshold Group (n:15; 10 females, 5 males), and Control Group (no stimulation) (n:16; 11 females, 5 males) according to the sensation of electrical current on ears. The participants were evaluated 3 times; before the application, after the first and second bicycle exercises. Numerical pain scale (NPS), pulse rate, blood pressure, respiratory rate, and distance traveled during exercise for sportive performance were recorded in kilometers as the evaluation method. The stimulation was done during the first bicycle exercise with 5 minutes of duration. The Kruskal-wallis, mann-whitney u test were used for the quantitative independent data obtained. In the analysis of qualitative independent data, chi-squared test was used.
Author: Sefa Haktan Atık
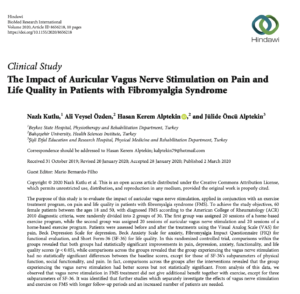
Title: The Impact of Auricular Vagus Nerve Stimulation on Pain and Life Quality in Patients with Fibromyalgia Syndrome
Abstract: The purpose of this study is to evaluate the impact of auricular vagus nerve stimulation, applied in conjunction with an exercise treatment program, on pain and life quality in patients with fibromyalgia syndrome (FMS). To achieve the study objectives, 60 female patients between the ages 18 and 50, with diagnosed FMS according to the American College of Rheumatology (ACR) 2010 diagnostic criteria, were randomly divided into 2 groups of 30. The first group was assigned 20 sessions of a home-based exercise program, while the second group was assigned 20 sessions of auricular vagus nerve stimulation and 20 sessions of a home-based exercise program. Patients were assessed before and after the treatments using the Visual Analog Scale (VAS) for pain, Beck Depression Scale for depression, Beck Anxiety Scale for anxiety, Fibromyalgia Impact Questionnaire (FIQ) for functional evaluation, and Short Form-36 (SF-36) for life quality. In this randomized controlled trial, comparisons within the groups revealed that both groups had statistically significant improvements in pain, depression, anxiety, functionality, and life quality scores (p < 0.05), while comparisons across the groups revealed that the group experiencing the vagus nerve stimulation had no statistically significant differences between the baseline scores, except for those of SF-36’s subparameters of physical function, social functionality, and pain. In fact, comparisons across the groups after the interventions revealed that the group experiencing the vagus nerve stimulation had better scores but not statistically significant. From the analysis of this data, we observed that vagus nerve stimulation in FMS treatment did not give additional benefit together with exercise, except for three subparameters of SF-36. It was identified that further studies which separately investigate the effects of vagus nerve stimulation and exercise on FMS with longer follow-up periods and an increased number of patients are needed.
Authors: Nazlı Kutlu, Ali Veysel Özden, Hasan Kerem Alptekin, Jülide Öncü Alptekin

Title: Extracellular and Intracellular Fluid Shifts on the Onset of Transcutaneous Auricular Vagus Nerve Stimulation
Abstract: In this paper, we propose multifrequency body impedance measurement technique for monitoring the onset of vagus nerve stimulation. In response to transcutaneous electrical vagus stimulation, changes occur in body fluids i.e. fluid shifts in extracellular and intracellular media that can be assessed by Cole parameters Re and Ri before and after stimulus, by measuring single side impedance spectroscopy (from 3 kHz to 1MHz) between wrist and ankle. Following a resting period of 5 minutes in supine position, auricular vagus nerve was stimulated for 3 minutes and BIS performed every 10 seconds, on 23-27 years old, 5 healthy subjects. During the stimulation phase, either an increase or a decrease was observed in extracellular and intracellular fluids. In 3 of the subjects, an ECF decrease of 0.02% per kg was compensated by 0.02 to 0.06% per kg increase in ICF; with a correlation coefficient of -0,70 to -0,79; suggesting fluid shifts between ECF and ICF. With the other 2 subjects, both ECF and ICF decreased by about 0.02% per kg. The study was performed with a limited number of participants; to reach statistically meaningful results measurements will be performed over a larger sample size.
Authors: Y. Ülgen, B. Büyüksaraç, B. Tunç and H. Solmaz