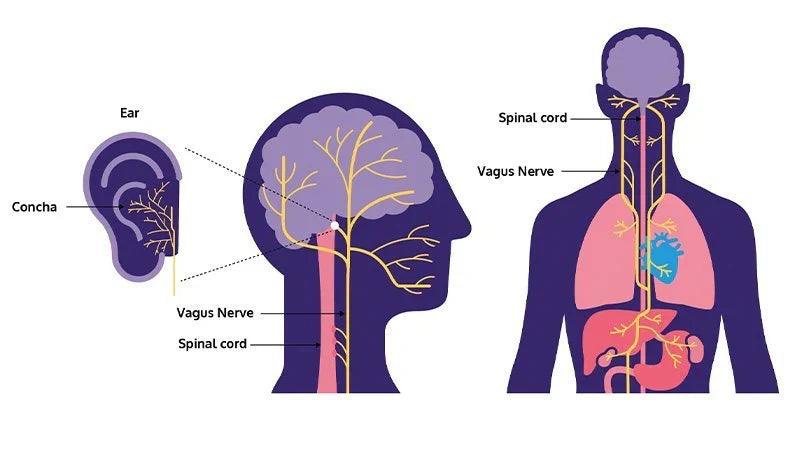
Background: The gut epithelium, derived from stem cells, is critical for maintaining gastrointestinal homeostasis. In ulcerative colitis (UC), the epithelial lining is compromised, leading to mucosal alterations and cell proliferation and differentiation disruptions. The therapeutic goal in UC management is to restore gut barrier function for sustained remission. The anti-inflammatory and protective properties of vagus nerve stimulation (VNS) can be delivered via non-invasive transcutaneous auricular VNS (NitaVNS).
Aims: To investigate the impact of NitaVNS on stem cell preservation, proliferative activity, and epithelial cell differentiation using a mouse model mimicking UC.
Methods: Male C57BL/6 mice received a 5-day regimen of 5% dextran sodium sulfate to induce colitis; control groups received regular water. Preventive NitaVNS or sham stimulation started one day before colitis induction and continued for six days. Disease activity index (DAI) was assessed daily, and macroscopic scores were determined upon sacrifice. Distal colonic markers associated with proliferating (leucinerich repeat-containing G-protein coupled receptor 5 [Lgr5]), fetal-like (lymphocyte antigen 6 A [Ly6A]), and quiescent (homeodomain-only protein homeobox [HOPX]) gut stem cells were evaluated using qRT-PCR and immunofluorescence (IF) expression patterns. Epithelial cell differentiation marker cytokeratin 20 (CK20), proliferation marker Ki67, gut-differentiated epithelial cells, tuft cell-associated doublecortin-like kinase 1 (DCLK1), and gobletcell-associated mucin2 (MUC2) were assessed.
Results: NitaVNS significantly ameliorated the DAI and macroscopic scores. In non- and colitic mice, no significant difference in the expression pattern was observed in HOPX and Ly6A and their respective colonic mRNA expression. Although NitaVNS decreased Lgr5 expression pattern and colonic mRNA expression in non-colitic mice, NitaVNS prevented the significant decrease in Lgr5 expression pattern and colonic mRNA expression in colitic mice. In sham colitic mice, CK20, Ki67, and MUC2 expression patterns decreased; however, NitaVNS prevented this deleterious effect. Per se, NitaVNS in non-colitic conditions did not show any effects. No effects were observed on mRNA expression. In sham-colitis mice, DCLK1 expression patterns and mRNA expression were decreased. However, NitaVNS prevented this deleterious effect in colitic mice. Per se, NitaVNS in non-colitic conditions did not show any effects.
Conclusion: NitaVNS preserves the proliferating stem cells responsible for tissue repair and maintains colonic proliferative activity, epithelial cell differentiation, and tuft and goblet cell-associated markers in colitic mice. Identifying the molecular mechanism underlying the protective role of NitaVNS may lead to novel therapeutic targets in UC.